VISIT THE FOLLOWING LINK FOR: TEST PRICES
Best Practices for Payment Collection
Our goal is to collect outstanding balances without sacrificing the quality of service. We want patients to feel supported while we follow a structured process. The walkdown is the rule—a proven set of steps we use to negotiate payments—but there will always be exceptions, especially when a patient is already aware of the prompt pay rate or is ready to make a payment.
Keep the Conversation Solution-Oriented
- Always aim to find a resolution, whether through Panam or Natera. Don’t let the patient go without guidance.
- Don’t push callers to the limit—listen carefully to their concerns and acknowledge their sentiment.
Under no circumstances should the patient be redirected to:
- Contact their clinic.
- Contact their insurance company.
- Be advised to retract or dispute a claim with the insurance.
Offer Payment Options Clearly
Approach the conversation using a top-down negotiation strategy.
- Prioritize sending the payment link when processing payments.
- Stay on the line to ensure the payment is completed.
- If the payment link is sent, inform the patient that it’s valid for 30 minutes after being opened.
Efficiency Matters
Guiding callers step by step through the process ensures not only payment success, but also a positive patient experience.
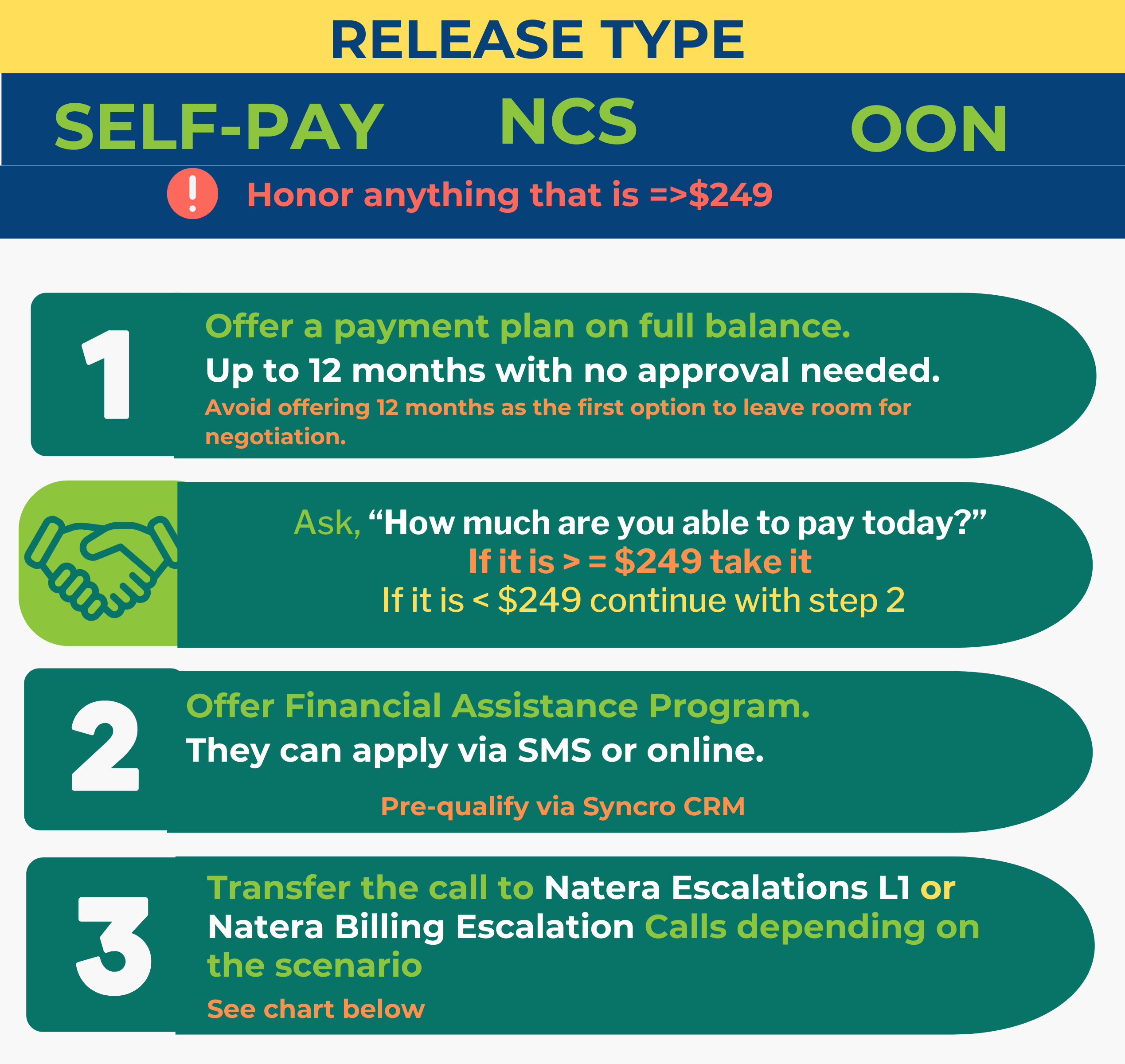
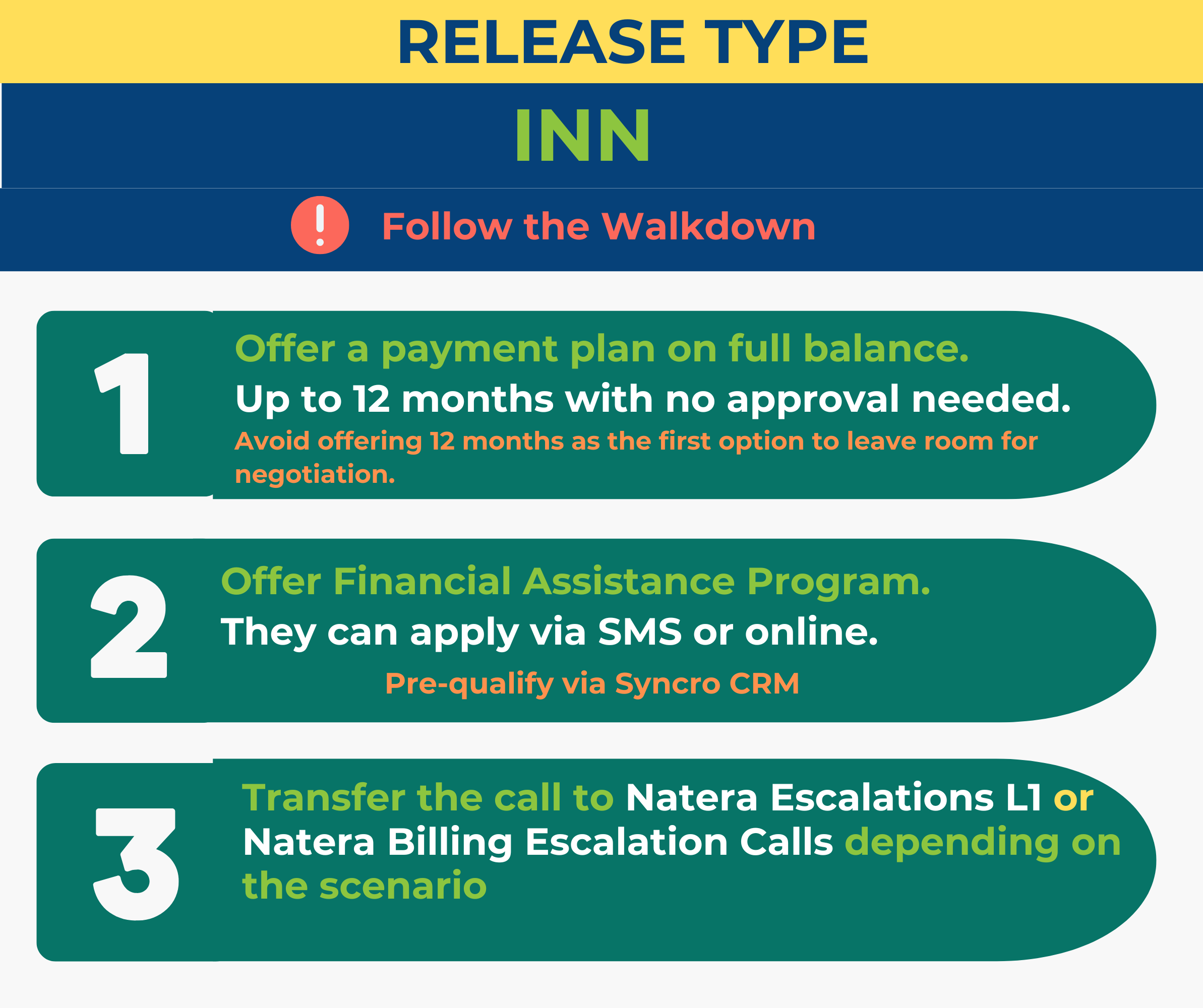
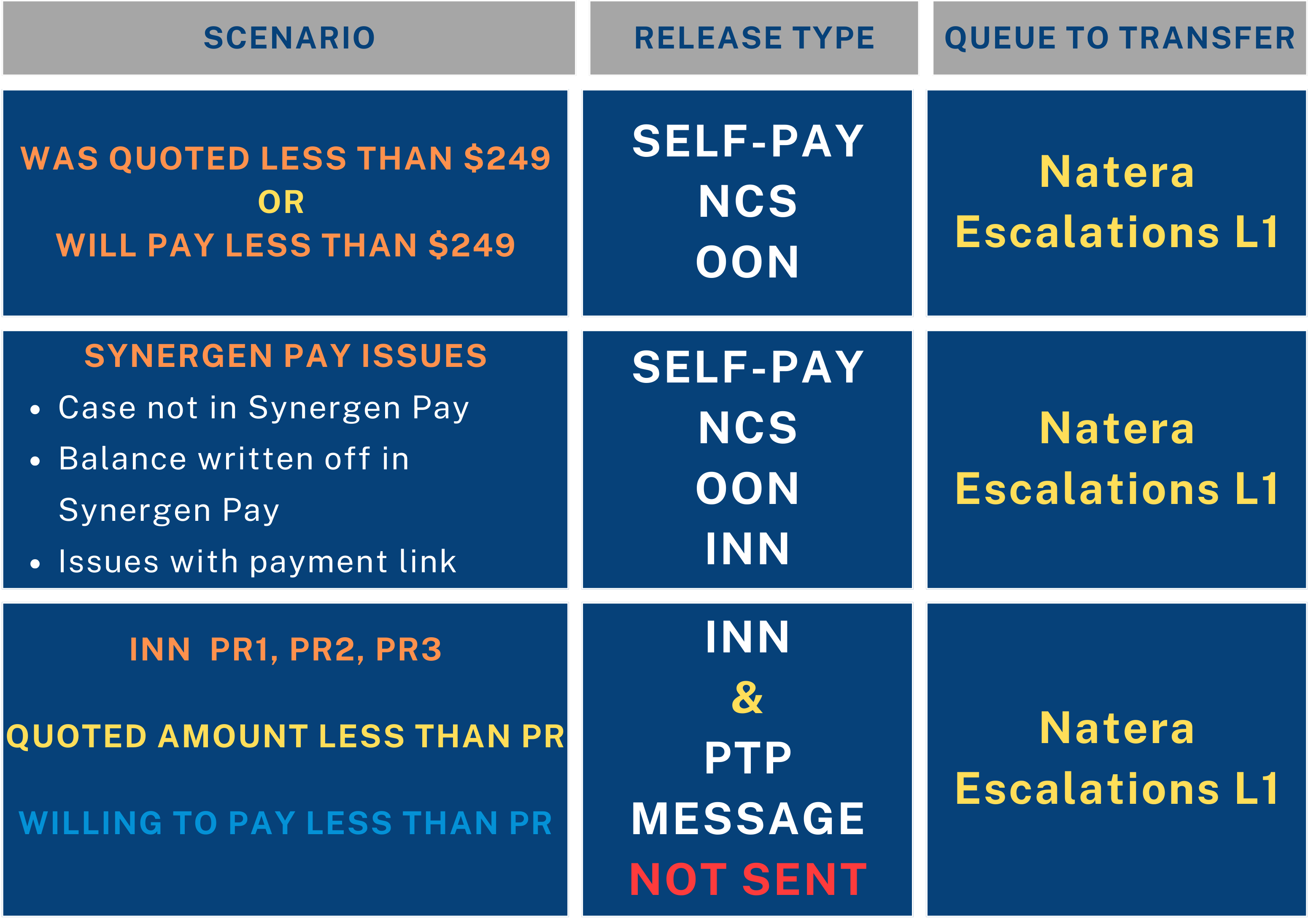
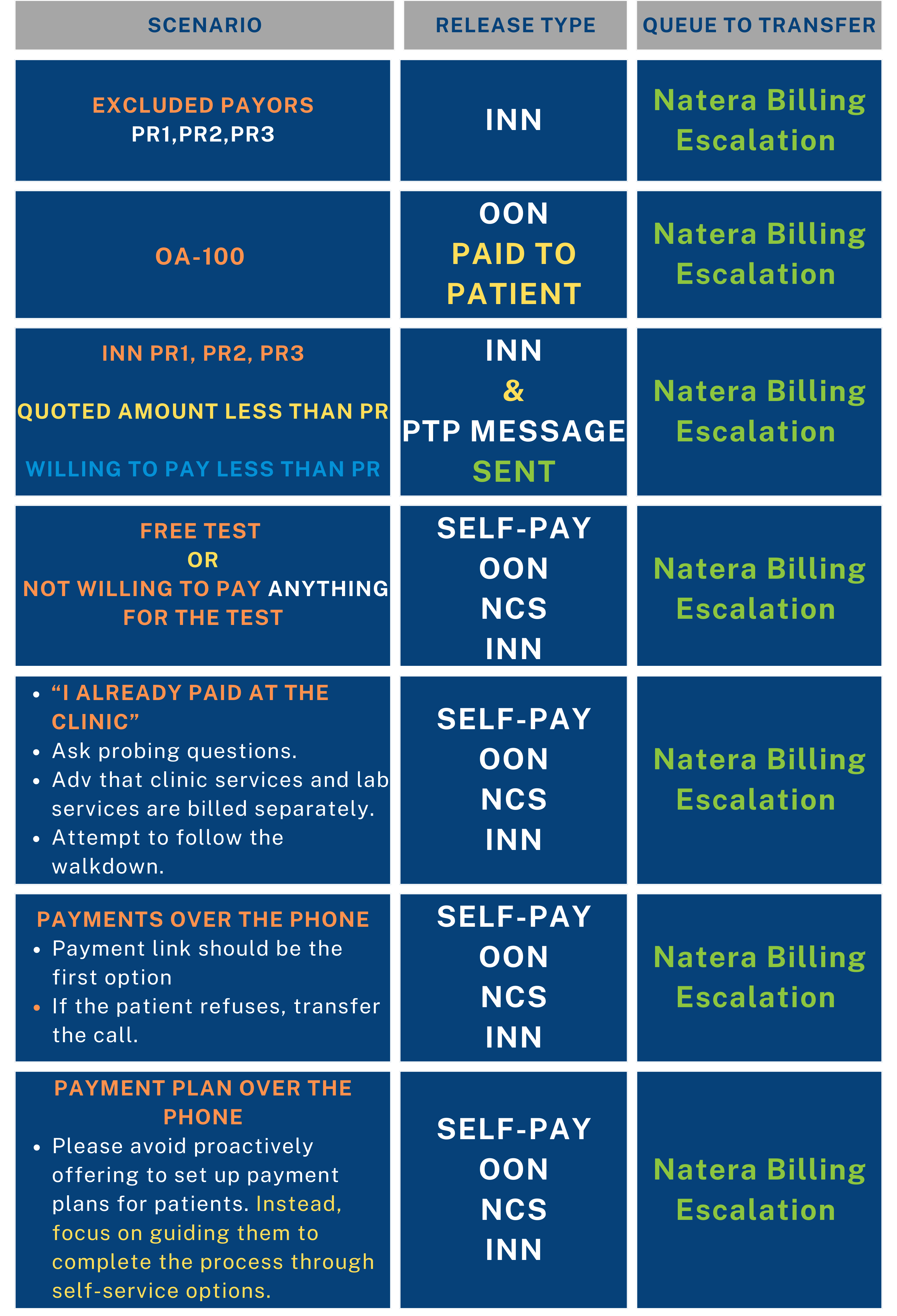
Walkdown Escalation Pathways
Always aim to negotiate, follow the walkdown process, and exhaust all available options.
This is a negotiation and a conversation—identify the right moment to escalate if necessary.
You can also refer to this KB Article if this comes up when negotiating with a caller Red Flags & Keywords
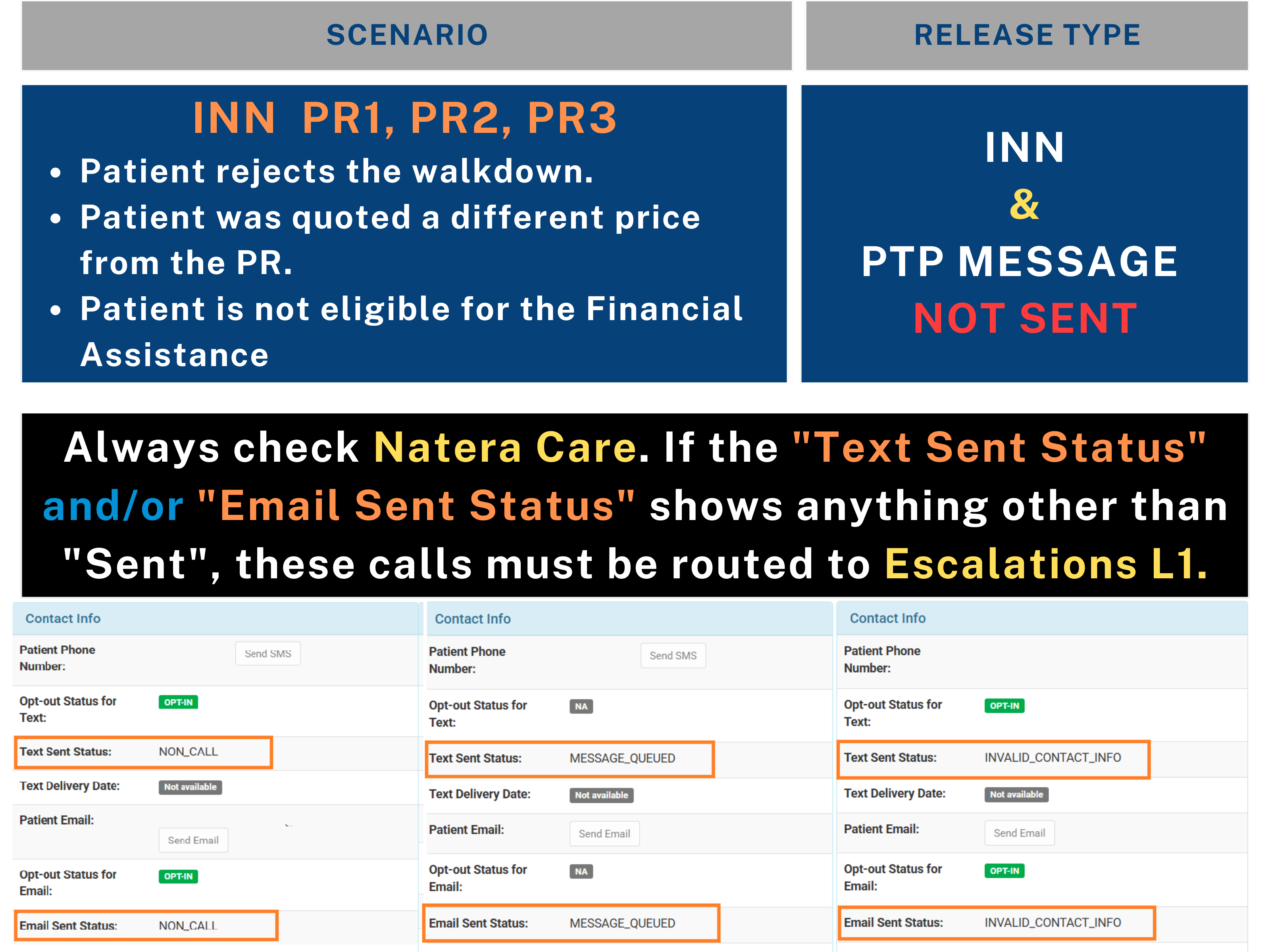
INN – PTP Message Not Sent
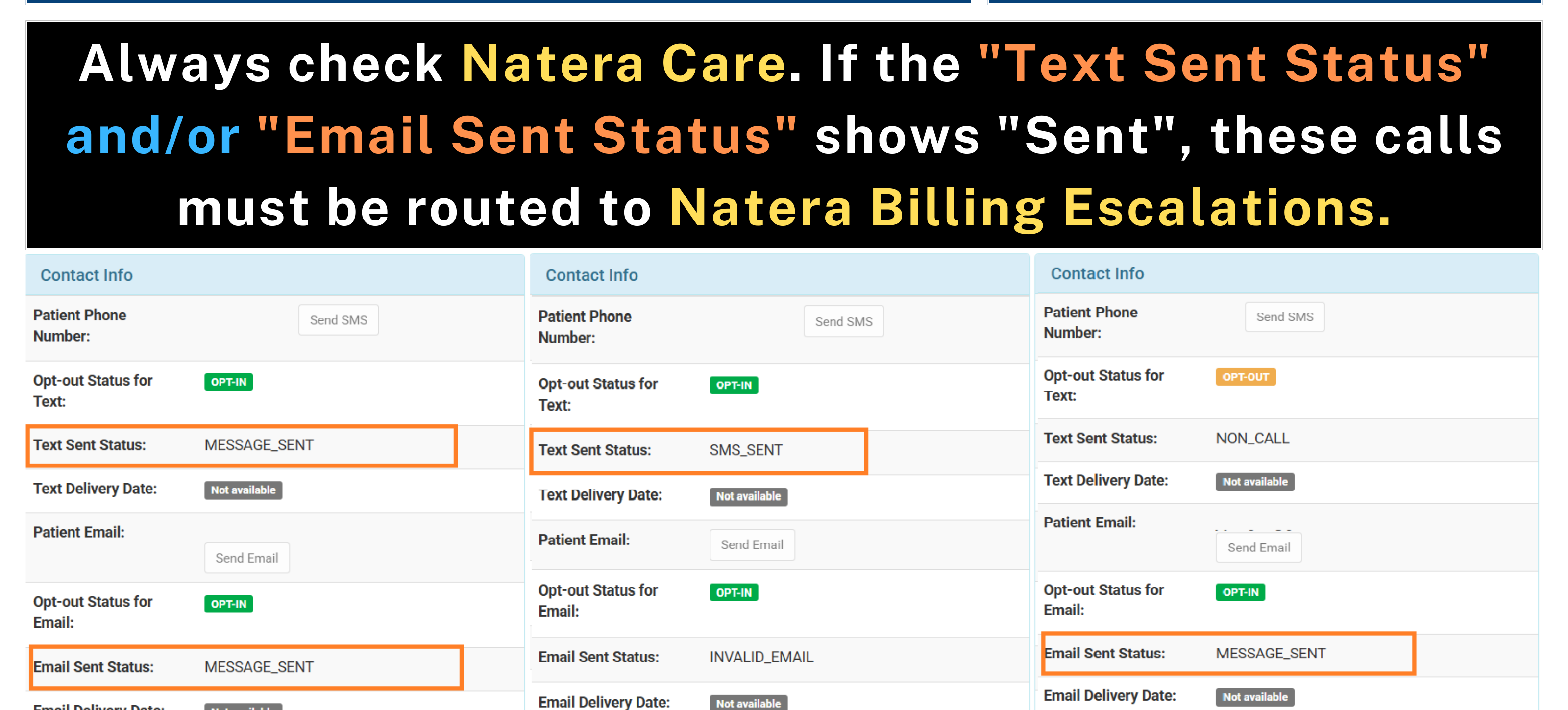
INN – PTP Message Sent
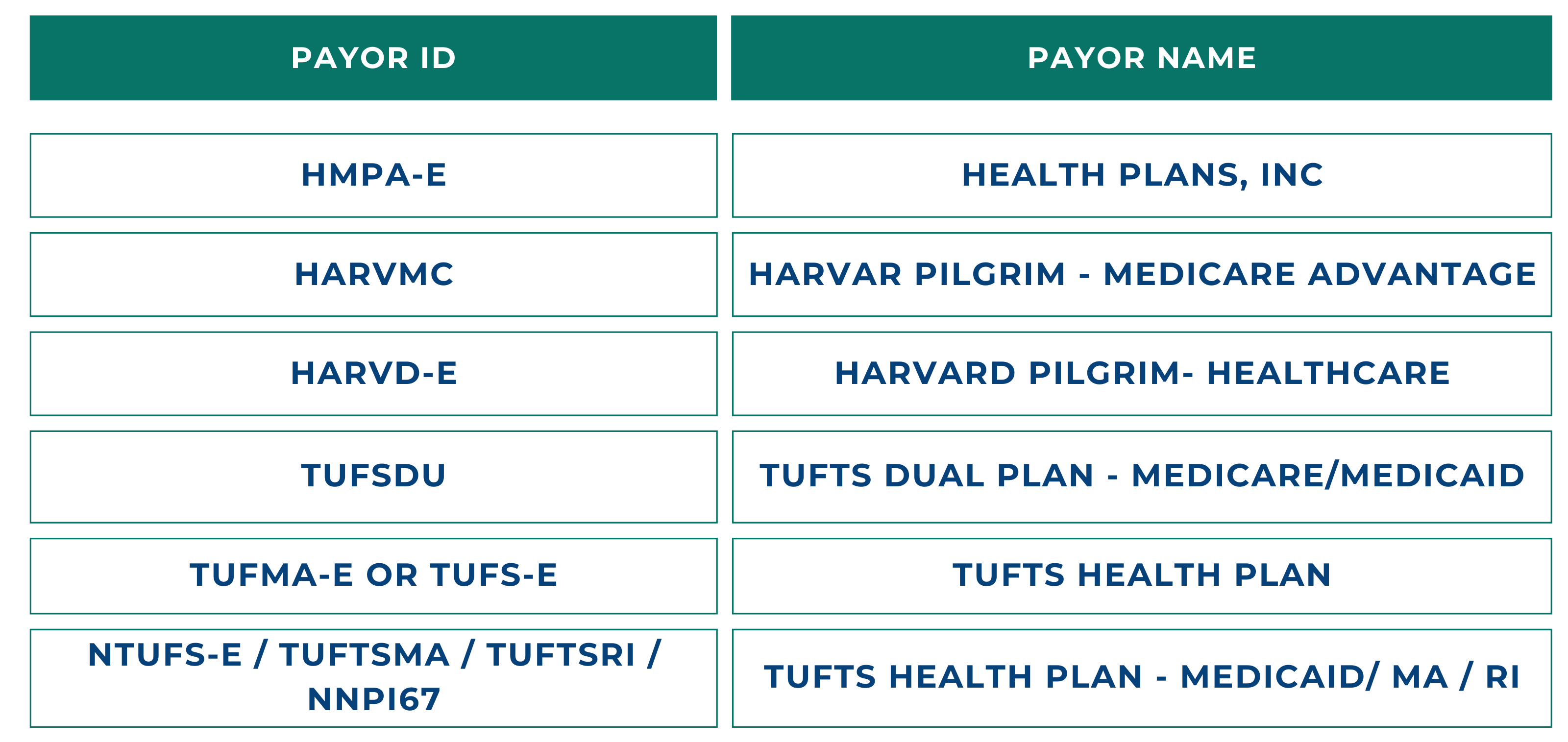
Excluded Payors
You will get a memo every time you pull a case that has an excluded payor.
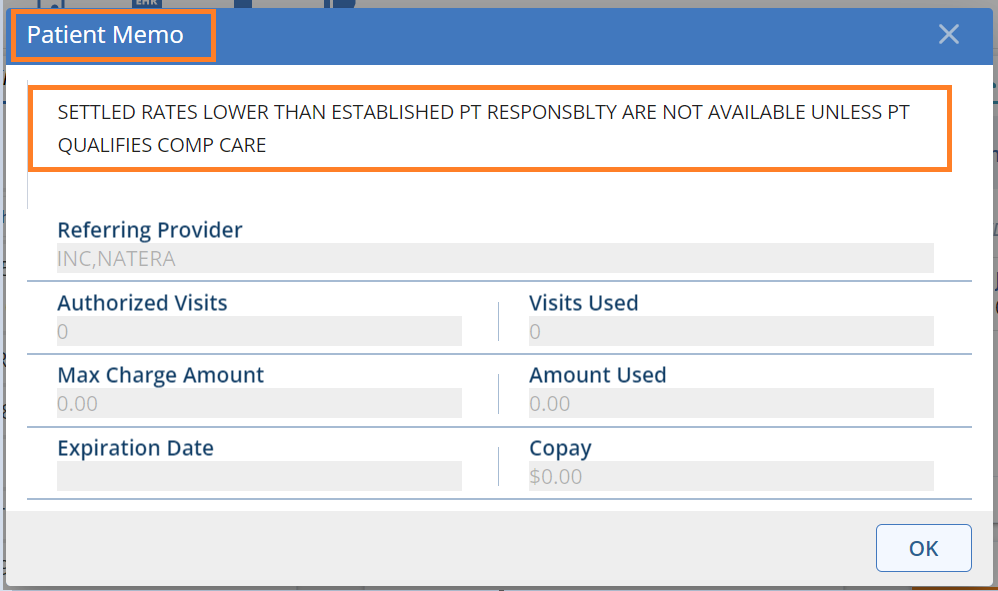
Billing reps follow the the walk down as a regular INN, must be transferred to Natera Billing Escalations if none of the WD options are of their interest.
Escalations L1 follow the walkdown as a regular INN , no courtesy exceptions should be applied
If the caller is not interested in any of the walkdown options, transfer to Natera Billing Escalations.
Use this script “We are unable to make any adjustments or exceptions to your balance. However, you may apply for our Compassionate Care program for financial assistance. Otherwise, the deductible, coinsurance, or copay amount determined by your insurance company will remain your responsibility.”
Attended Transfer
Queue Name: Natera Escalations L1
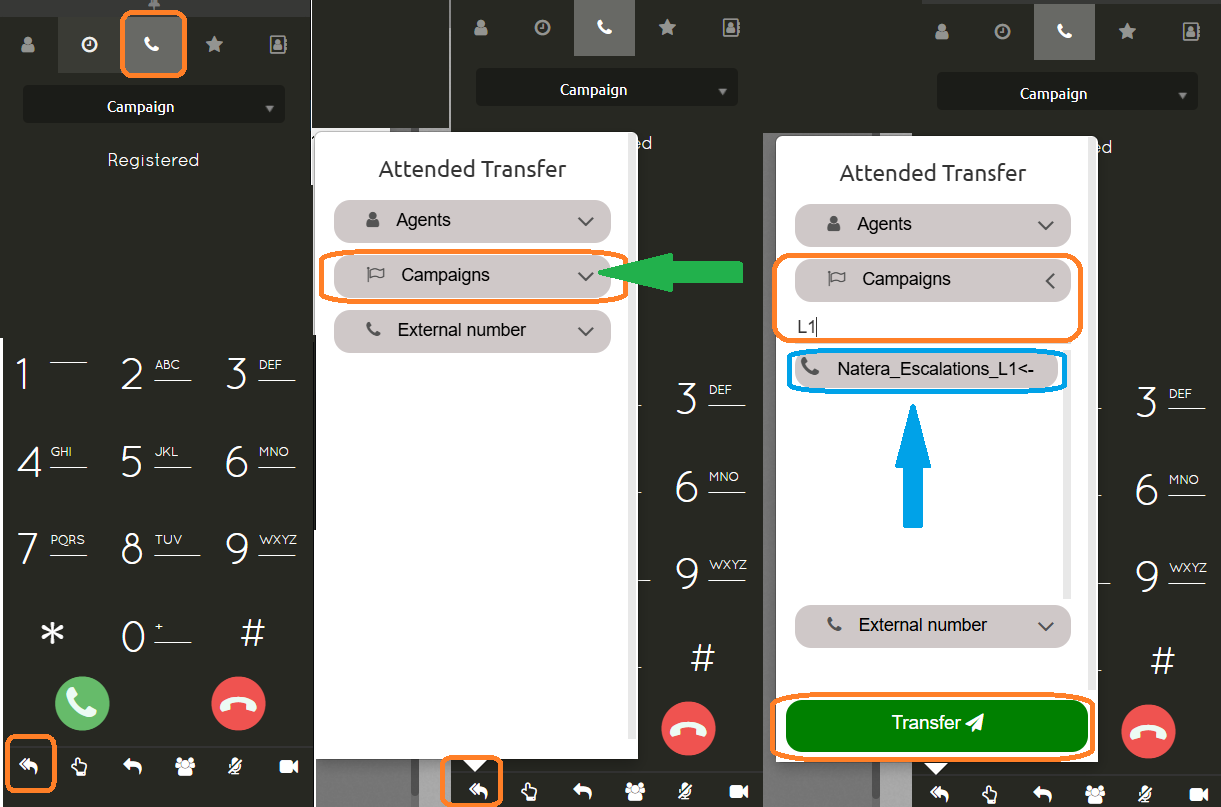
Attended Transfer
Queue Name: Natera Billing Escalations
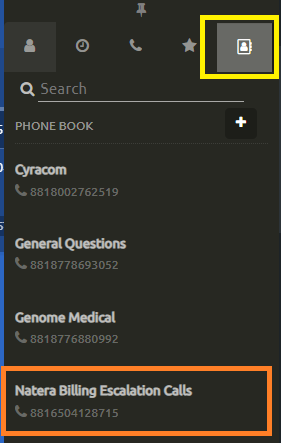
From the Phone Book
Documenting Walkdown options offered
Record essential information: When you are unable to follow or offer the complete walkdown process fully, it’s important to notate which steps were presented to the patient accurately.
This ensures transparency and helps us maintain clear records for each interaction.
If all options were offered but the patient was not interested, you should notate something like: “All walkdown options offered, but patient declined.”
If you were able to offer only certain steps, for example, just the payment plan, please make sure to notate: “Payment plan offered.”
Related Topics:
OON Bills
When to send a Zbal
Payments in Synergen
Payment Plan for Signatera Only
Last update by: Nina O (Feb 12, 2025)