Digital Statements Update
Digital Only Outreach for Patients with a Bad Address in AMD:
We have a new process that will allow us to send a text or email to patients letting them know they have a bill due if we do not have their address to send a physical statement in the mail. (Bad address).
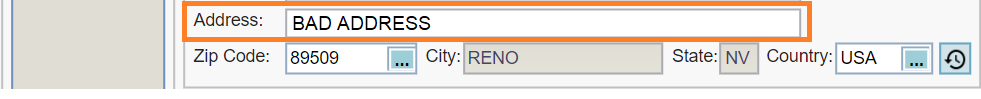
PanAm went live with the process on 04/12/2024, and any patient to whom we were able to send a Digital Only Statement will have the following in AMD under the Release type:
- DIGITAL INN
- DIGITAL OON
- DIGITAL SF
- DIGITAL NCS
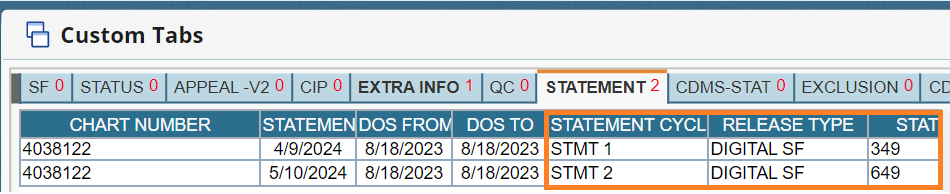
Place a statement hold and submit a Syncro CRM Demographics Update ticket to get the patient’s address corrected/updated.
Make sure you ADD a new line after the latest statement 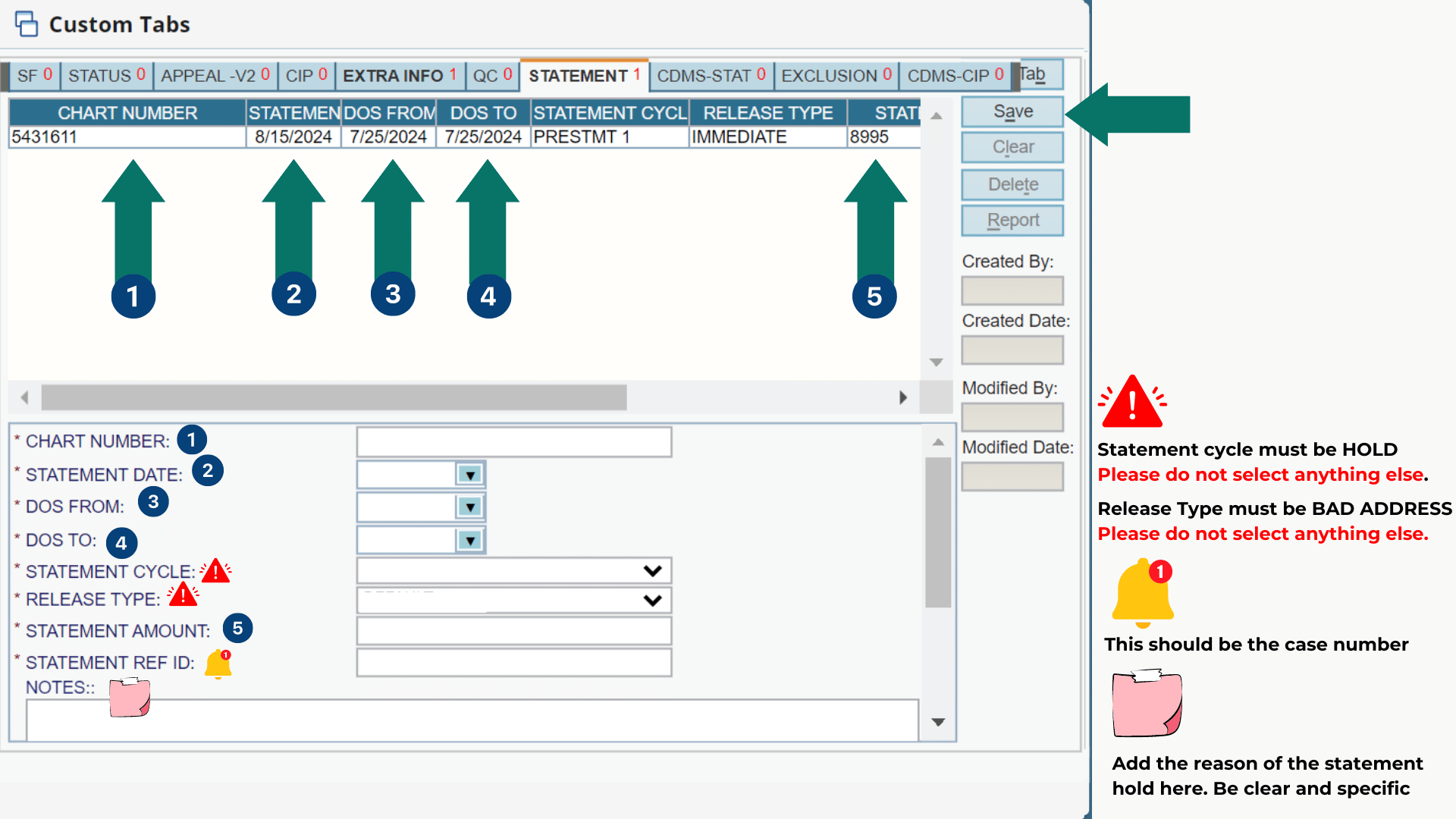
Note: If the patient has a combo case (Two different case numbers), you must place a Hold and follow the same process for each case.
CSS Responsibility: Once the CSS receives the Syncro CRM ticket, they MUST update/correct the patient’s address and email Synergen SOS asking to restart the Standard Dunning Cycle for the case. We want to ensure the patient doesn’t lose the prompt pay discount by sending Statement 2 vs Statement 1.
If the patient processes a payment, DO NOT place a Statement Hold. Instead, submit a Syncro CRM Demographics Update ticket to have the patient’s address corrected or updated.
MEDICAID Write Off
If the patient receives a billing statement because their STRAIGHT MEDICAID insurance did not cover the test. In that case, they should not be held responsible for payment if their MEDICAID insurance did not cover it.
Place a hold on the statement by selecting Statement Cycle = HOLD, and the required release type is NCS.
- In AMD, Custom Tabs
- Statement Tab – Validate DOS
- ADD a new line with a Hold after the latest statement – Everything must match from the previous statement line and only change the cycle hold
- Put in the chart number
- the statement date
- the DOS from and To
- the statement cycle = HOLD
- release type = NCS
- statement amount and
- case# (statement ref ID)
- Save
Once the Syncro CRM escalation has been sent it will take 5-7 business days to have the patient’s balance written off.
If Straight Medicaid denied a claim due to Timely Filing, the balance will be written off after you send a Synergen Escalation through SyncroCRM (Ensure the patient had Medicaid coverage at the DOS)
If the patient is receiving bills after processing a Medicaid insurance update and the TAT is already exceeded, please check the statement generation date to verify if it was generated before the process was completed, send a Synergen Escalation through SyncroCRM, so we can submit a Medicaid Eligibility Review.
Last update by: Nina O (Feb 20, 2025)