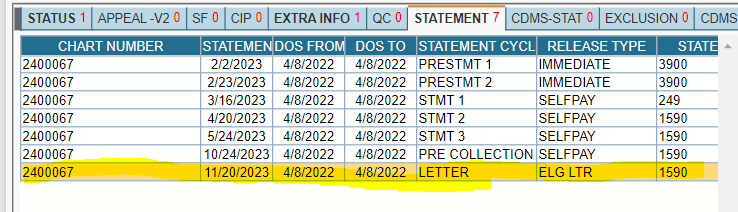
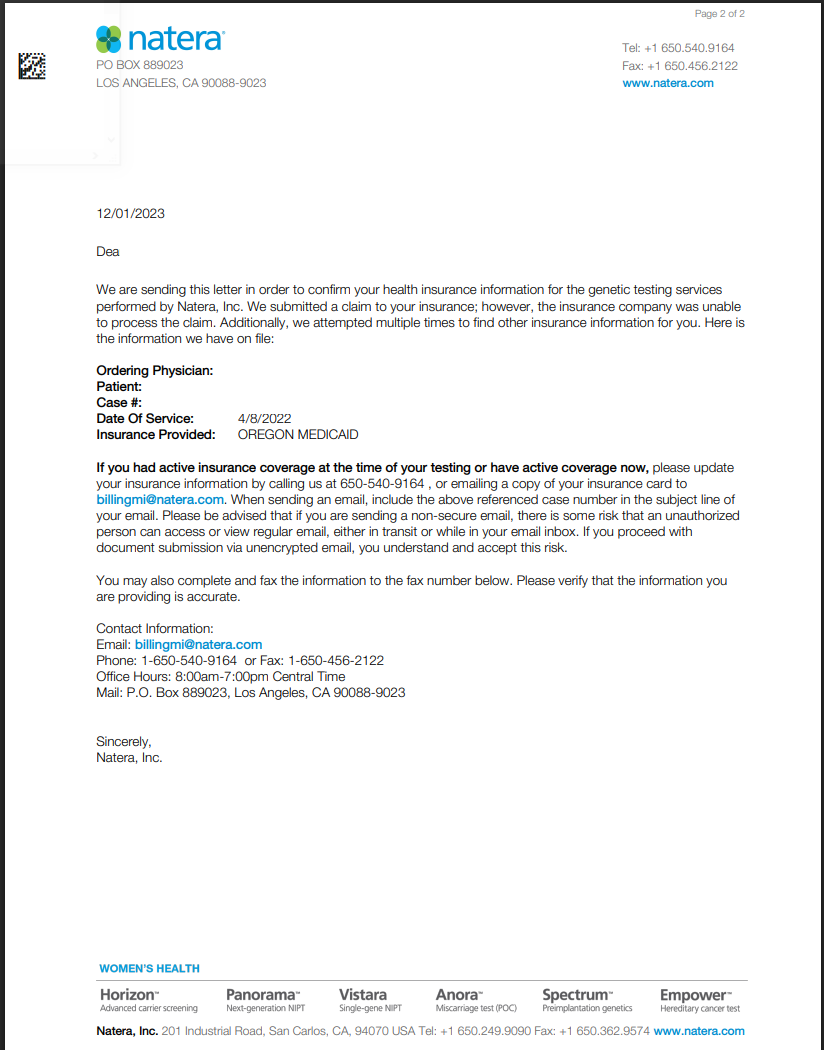
This is sent to patients when a claim was submitted to their registered insurance, but we were unable to process it—either Pre-Statement 1 Immediate or Pre-Statement 2 Immediate.
- We typically place a hold on statements while waiting for a response from the patient.
- Collect the patient’s insurance information and submit a “Synergen Escalation” via Syncro CRM, advising the patient to allow 30–45 business days for processing.
- If the patient did not have active coverage on the date of service (DOS), follow the walkdown process.
- If the patient insists on submitting the claim to insurance, explain that it is unlikely to be processed, but submit a “Synergen Escalation” via Syncro CRM and advise the patient to wait 30–45 business days.
Last update by: Nina O (March 14,2025)