Out-of-Network (OON) Insurance Payment Process
Insurance Payments to Natera: Out-of-Network (OON) insurance companies may need to send a check to Natera for their portion of the claim.
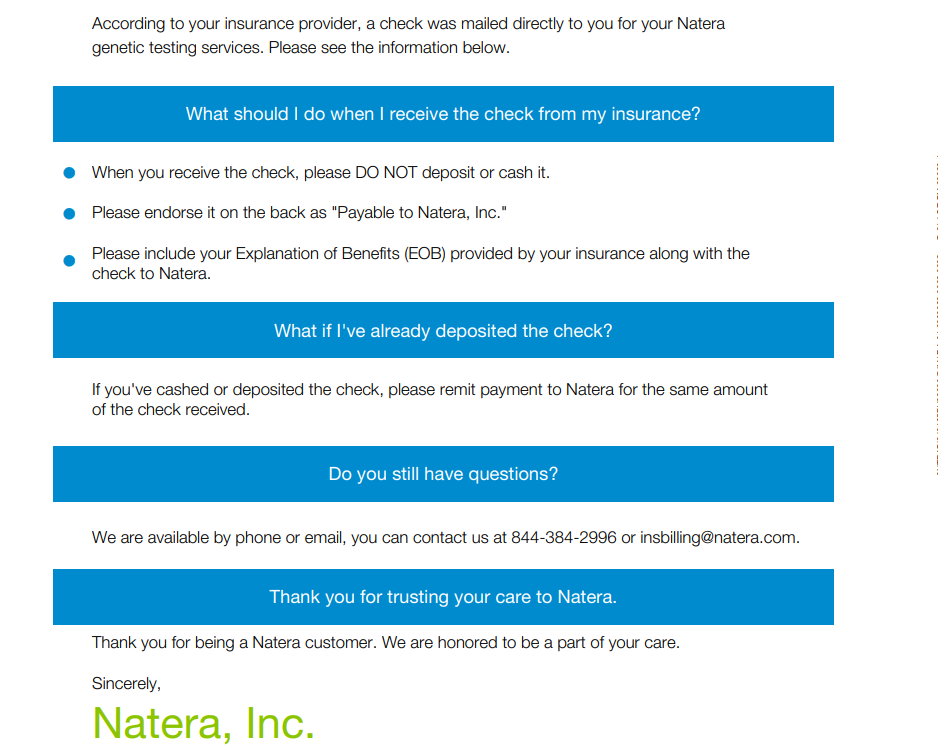
Patient-Received Checks: Since the plan is OON, insurance cannot send the check directly to Natera. Instead, the check will be sent to the patient. Once received, the patient must endorse the check to Natera and mail it to: P.O. BOX 889023, Los Angeles, CA 90088-9023
Processing Time: Please note that it takes approximately 30 to 45 business days for a mailed check to be processed.
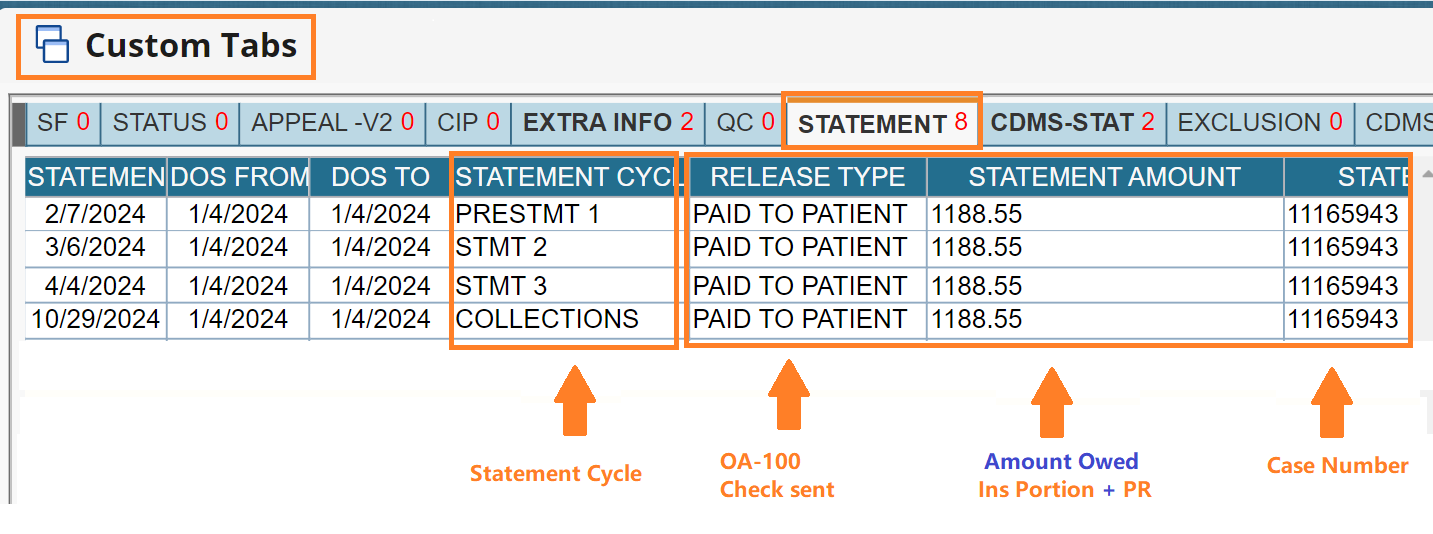
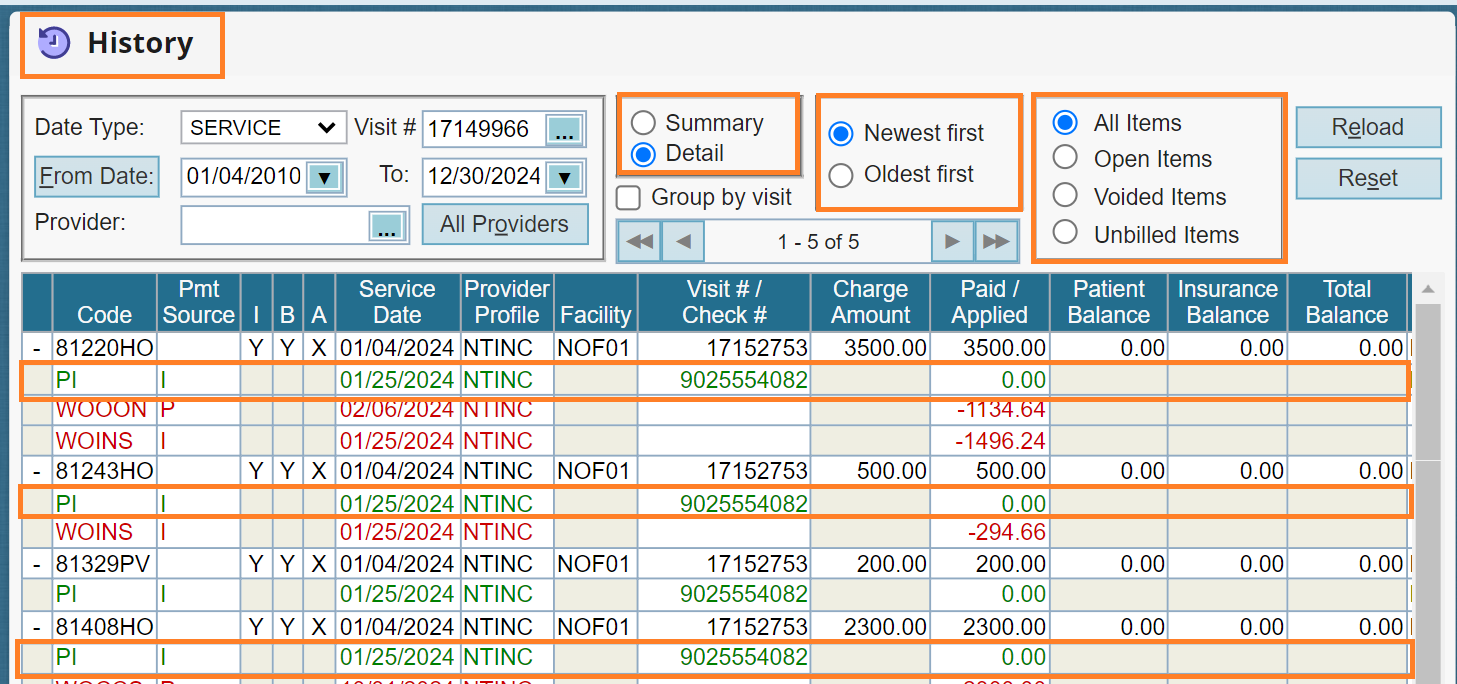
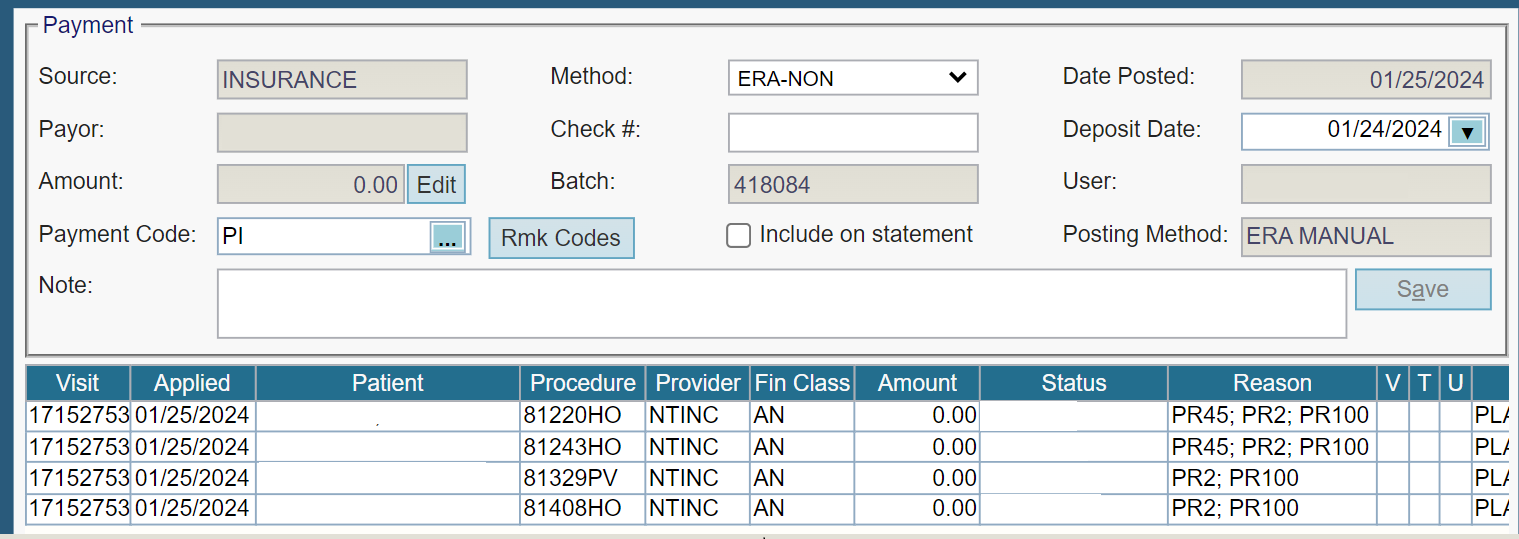
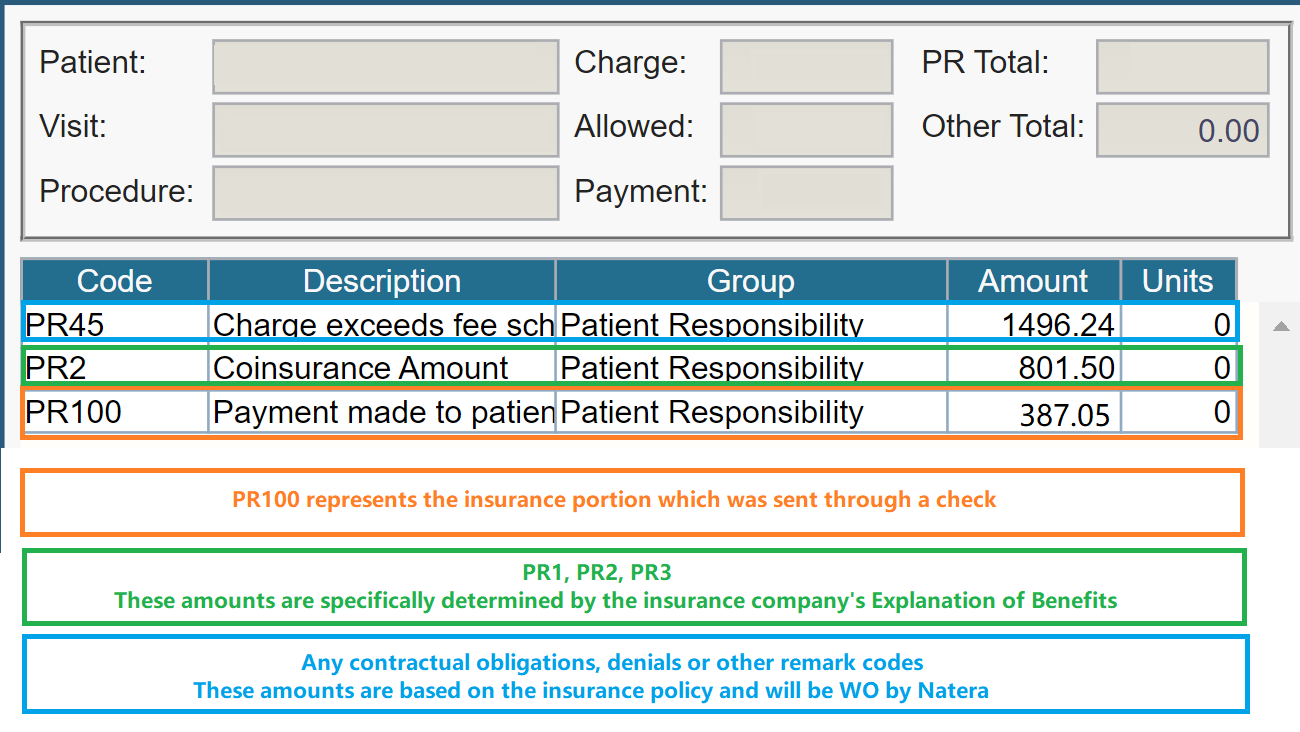
Identifying OA100 Checks: You can verify if a case has an OA100 check by reviewing the Reason Codes in the History tab, where it will appear under the code OA100 or PR100.
Patient Responsibility (PR): In addition to the insurance check, there is often a Patient Responsibility amount.
OA-100 Statement Cycle
Before sending billing statements, Natera will send a pre-statement notification letter to notify the patient of an OA-100 check issued by their insurance provider. These letters are known as PR 100 letters by Natera.
Important Guidelines for OA100 Checks
Do not offer any discounts or Compassionate Care on OA100 check amounts.
Compassionate Care or Courtesy Exceptions apply only to the Patient Responsibility portion.
Patients may apply for Compassionate Care if:
> They have paid the OA100 amount in full.
> They have not yet covered their Patient Responsibility.
> There is an outstanding balance.
In these cases, Compassionate Care assistance may apply to the remaining unpaid balance.
Collections Process for OA100
If payment is not received within the first 3 billing cycles, the account will be forwarded to an external collections agency.
At this stage, patients must contact the agency directly to arrange payment.
CCS (External Collections’ Agency)
Phone: 800-697-2767
Monday–Friday: 8:00 AM – 8:00 PM EST
Saturday: 9:30 AM – 5:00 PM EST
If a Patient Did Not Receive the Check
Advise patients to send their complete EOB to [email protected] and then call back.
If they do not have the EOB, ask them to contact their insurance provider to request it.Once they receive the EOB, they should send it to [email protected] and then call back.
FAQs
Can patients have the option to deposit the check into their account and pay the OA-100 + their PR over the phone? Yes, they can.
If patients decide to pay the OA-100 by sending a check, how could they pay the PR? We need to wait to receive the check and confirm the payment is posted before processing the PR payment (whether through a payment plan or by honoring a rate).
Are there any guidelines for paying the OA-100? Specifically, must the OA-100 always be paid first, or can the patient pay their PR first?
The PR100 must be paid first or processed in parallel. Patients cannot pay the PR before the OA-100.
Last update by: Nina O(Apr 11, 2025)